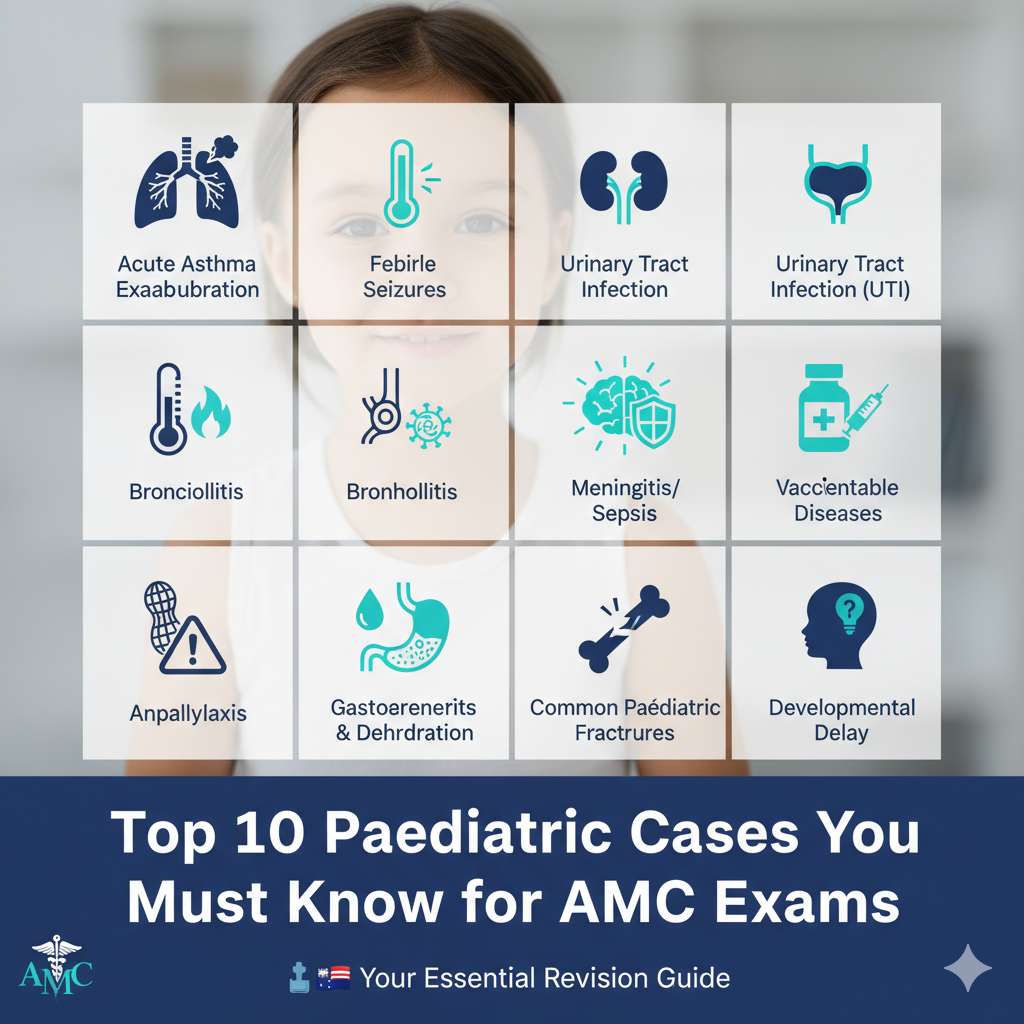
Top 10 Paediatric Cases You Must Know for AMC Exams 🩺
Hey future AMC superstars! Paediatrics can be a challenging yet incredibly rewarding section of your exams. To help you ace it, I’ve compiled a list of the top 10 paediatric cases that frequently appear in the AMC and are essential to master. Understanding these conditions, their presentation, management, and potential complications will give you a significant edge. Let’s dive in!
1. Acute Asthma Exacerbation 🌬️
Why it’s crucial: Asthma is very common in children, and recognizing and managing acute exacerbations is a core competency.
- Key features: Wheezing, cough, shortness of breath, accessory muscle use, and prolonged expiratory phase. Severity assessment is vital (mild, moderate, severe, life-threatening).
- Management: Salbutamol (SABA) via spacer, corticosteroids (oral or IV), oxygen, ipratropium bromide.
- AMC tip: Focus on the step-wise management approach and when to escalate care.
2. Febrile Seizures 🔥
Why it’s crucial: These are common and can be very distressing for parents. Knowing how to differentiate simple from complex febrile seizures is key.
- Key features: Seizure occurring with fever (>38°C) in a child aged 6 months to 5 years, without central nervous system infection or other metabolic cause.
- Management: Primarily supportive. Antipyretics for comfort, education for parents.
- AMC tip: Understand the criteria for simple vs. complex and when to investigate further (e.g., lumbar puncture).
3. Bronchiolitis 🦠
Why it’s crucial: A common respiratory infection in infants, often caused by RSV.
- Key features: Prodrome of upper respiratory tract symptoms, followed by cough, tachypnoea, wheezing, crackles, and increased work of breathing. Most severe in infants under 6 months.
- Management: Supportive care – hydration, nasal suctioning, oxygen if hypoxic. Bronchodilators and steroids are generally not recommended.
- AMC tip: Emphasize the supportive nature of management and the limited role of medications.
4. Gastroenteritis and Dehydration 💧
Why it’s crucial: Diarrhoea and vomiting are common in children, and dehydration can be life-threatening if not recognized and managed promptly.
- Key features: Vomiting, diarrhoea, fever, abdominal pain. Assess severity of dehydration (mild, moderate, severe) using clinical signs (e.g., sunken fontanelle, decreased urine output, dry mucous membranes, prolonged capillary refill time).
- Management: Oral rehydration solution (ORS) is the cornerstone. IV fluids for severe dehydration or intractable vomiting.
- AMC tip: Practice calculating fluid requirements and understanding the different phases of IV fluid rehydration.
5. Anaphylaxis 🥜
Why it’s crucial: A medical emergency requiring immediate recognition and treatment.
- Key features: Acute onset of skin and/or mucosal changes (hives, angioedema), plus respiratory compromise (wheeze, stridor) and/or reduced blood pressure/collapse.
- Management: Adrenaline (epinephrine) IM is the first-line treatment. Call for help, maintain airway, oxygen.
- AMC tip: Know the correct dose and route of adrenaline for different age groups and the importance of prompt administration.
6. Urinary Tract Infection (UTI) 🚽
Why it’s crucial: UTIs are common and can lead to renal scarring if not treated effectively, especially in younger children.
- Key features: Fever, irritability, poor feeding in infants. Dysuria, frequency, urgency, abdominal pain, enuresis in older children.
- Diagnosis: Urine dipstick, urine microscopy and culture (MSU or catheter sample/suprapubic aspirate for infants).
- Management: Antibiotics (oral or IV depending on severity and age). Consider renal ultrasound and MCUG for recurrent UTIs.
- AMC tip: Understand appropriate urine collection methods for different ages and indications for imaging.
7. Meningitis/Sepsis in Infants 🧠
Why it’s crucial: These are life-threatening conditions where early diagnosis and aggressive management are critical.
- Key features: Non-specific symptoms in infants (fever, irritability, poor feeding, lethargy, bulging fontanelle, hypotonia). Older children may have classic signs (neck stiffness, photophobia, rash).
- Diagnosis: Blood tests (FBE, CRP, blood culture), lumbar puncture.
- Management: Empirical broad-spectrum IV antibiotics immediately, often before definitive diagnosis. Supportive care.
- AMC tip: Emphasize the urgency of treatment and the high index of suspicion required in febrile infants.
8. Common Paediatric Fractures (e.g., buckle, greenstick) 🦴
Why it’s crucial: Children’s bones are different! Understanding common fracture patterns and their management is important.
- Key features: Pain, swelling, deformity, inability to use the limb after trauma.
- Diagnosis: X-ray.
- Management: Immobilization (cast, splint). Recognize signs of child abuse in suspicious fractures.
- AMC tip: Know the different types of paediatric fractures and the Salter-Harris classification for growth plate injuries.
9. Developmental Delay 🤔
Why it’s crucial: Early identification and intervention are key for improving outcomes.
- Key features: Failure to meet age-appropriate developmental milestones in one or more domains (gross motor, fine motor, speech/language, social/personal, cognitive).
- Assessment: Detailed history, physical examination, developmental screening tools.
- Management: Referrals to appropriate specialists (e.g., paediatrician, speech therapist, occupational therapist, physiotherapist).
- AMC tip: Be familiar with key developmental milestones and red flags for referral.
10. Vaccine-Preventable Diseases 💉
Why it’s crucial: Understanding the Australian immunization schedule and the presentation of these diseases is fundamental.
- Key features: Recognize measles (maculopapular rash, Koplik spots), mumps (parotitis), rubella (mild rash, lymphadenopathy), pertussis (whooping cough), chickenpox (vesicular rash).
- Management: Mostly supportive, but prevention through vaccination is paramount.
- AMC tip: Know the standard Australian immunization schedule and be able to counsel parents on vaccine hesitancy.
Final Thoughts for Your AMC Journey 🚀
Mastering these top 10 paediatric cases will provide a strong foundation for your AMC exams. Remember to:
- Practice with vignettes: Apply your knowledge to clinical scenarios.
- Understand pathophysiology: Knowing “why” helps you remember “what.”
- Focus on management plans: This is where many marks are gained or lost.
- Be confident: You’ve got this!
Good luck with your studies, and keep that dedication burning bright! If you have any questions or want to discuss specific cases, feel free to drop a comment below.
